Ulcerative Colitis Treatment: Managing a Chronic Inflammatory Bowel Disease
Ulcerative colitis (UC) is a chronic inflammatory bowel disease that primarily affects the lining of the large intestine (colon) and rectum. It manifests as periods of remission interspersed with flare-ups of symptoms. Effective management of ulcerative colitis is crucial to reduce symptoms, achieve long-term remission, and improve quality of life. This guide provides insights into current treatment options, lifestyle adjustments, and coping strategies for ulcerative colitis.
Understanding Ulcerative Colitis
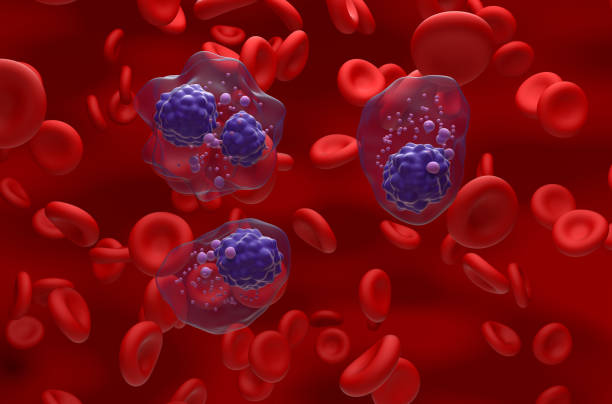
Ulcerative colitis is characterized by inflammation and sores (ulcers) in the lining of the colon and rectum. Symptoms include abdominal pain, bloody diarrhea, fatigue, and weight loss. The exact cause is unknown, but it involves an abnormal response of the immune system.
Treatment Goals for Ulcerative Colitis
- Reduce Symptoms: Alleviate the symptoms of UC, including pain and diarrhea.
- Induce and Maintain Remission: Reduce the frequency and severity of flare-ups.
- Prevent Complications: Such as colon cancer and other conditions related to UC.
Medications for Ulcerative Colitis
Aminosalicylates
- Used for mild to moderate symptoms, these drugs reduce inflammation in the colon.
Corticosteroids
- For more severe symptoms, steroids can quickly reduce inflammation but are not suitable for long-term use due to side effects.
Immunomodulators
- Modify the immune system response to decrease inflammation. They are often used when other medications are ineffective.
Biologics
- Target specific pathways in the immune system to reduce inflammation. Administered via infusion or injection.
Janus Kinase (JAK) Inhibitors
- A newer class of oral medications that block certain immune responses.
Dietary and Lifestyle Management
- Diet Adjustments: Identify and avoid foods that trigger symptoms.
- Nutrition: Ensure a balanced diet to compensate for nutrient deficiencies.
- Hydration: Increased fluid intake, especially during flare-ups.
- Stress Management: Stress can exacerbate UC symptoms, so stress-reduction techniques are beneficial.
Surgical Options
- In severe cases, or if there’s a risk of cancer, surgery to remove part or all of the colon may be necessary.
Managing Flare-ups
- Recognizing early signs of a flare-up and adjusting treatment accordingly.
- Regular communication with healthcare providers for timely intervention.
Alternative Therapies
- Some patients find relief with complementary therapies like acupuncture, probiotics, or herbal remedies, though these should not replace conventional treatment.
Coping and Support
- Joining support groups for people with ulcerative colitis.
- Psychological support or counseling to help cope with the emotional aspects of living with a chronic condition.
Regular Monitoring and Check-ups
- Regular colonoscopies and screenings for colon cancer.
- Ongoing assessment of treatment effectiveness and adjustment as needed.
Conclusion
Ulcerative colitis is a lifelong condition that requires ongoing management through a combination of medication, diet, lifestyle adjustments, and, in some cases, surgery. While there is no cure, effective treatment can help manage symptoms, reduce the occurrence of flare-ups, and maintain remission. Working closely with healthcare providers and adopting a proactive approach to treatment and lifestyle changes can significantly improve the quality of life for individuals with ulcerative colitis.